Lipids & Longevity: Optimize Your Healthspan
- Marcus Reed
- Health , Longevity , Cardiovascular , Nutrition
- May 27, 2025
Table of Contents
Fast Facts: Lipoproteins & Your Health (TL;DR)
- LDL Cholesterol: Aim for <100 mg/dL (general) or <70 mg/dL (high-risk); lower is often better for preventing heart disease.
- HDL Cholesterol: While ‘good,’ its direct protective role is complex; focus on overall lifestyle, not just raising HDL numbers.
- Lipoprotein(a) [Lp(a)]: A genetic risk factor for heart disease; levels are stable and a one-time test can reveal your risk.
- Apolipoprotein B (apoB): A comprehensive measure of ‘bad’ cholesterol particles; <80 mg/dL is a common target.
- Actionable Steps: Diet, exercise, and targeted medications (if needed) are key to managing lipoproteins for a longer, healthier life.
Optimizing Your Lipoproteins: A Cornerstone of Longevity and Healthspan
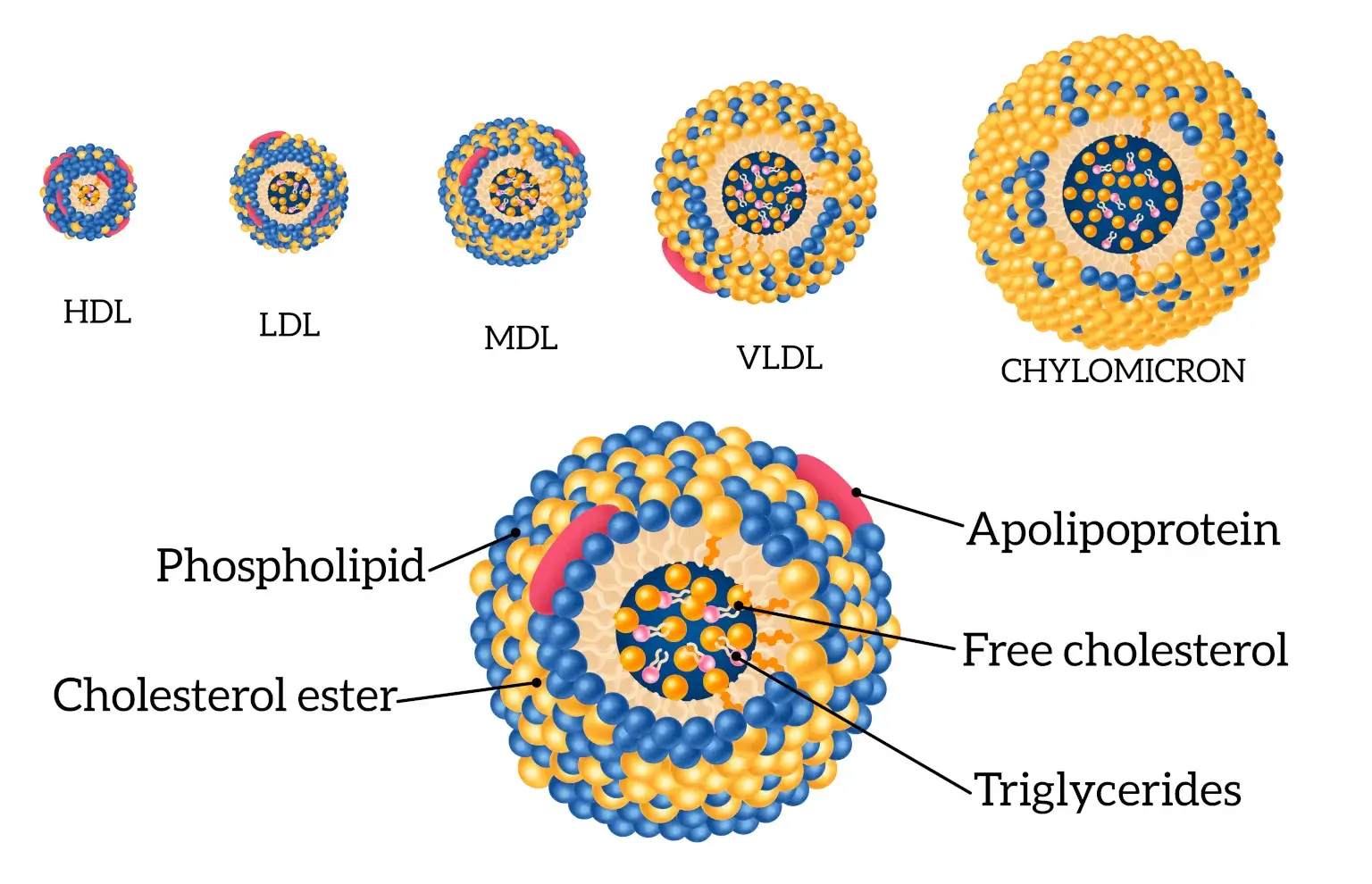
Our pursuit of a long, energetic, and fulfilling life—often referred to as healthspan—is closely linked to the condition of our cardiovascular system. At the heart of cardiovascular health are lipoproteins, the complex particles that transport cholesterol and fats through our blood. Among the most influential of these are Low-Density Lipoprotein (LDL), High-Density Lipoprotein (HDL), Lipoprotein(a) [Lp(a)], and Apolipoprotein B (apoB). These markers don’t just shape our risk for heart disease—they play a pivotal role in determining both the length and quality of our lives.
By gaining a deeper understanding of these lipoproteins and their functions, we can make informed choices that enhance longevity and vitality.
LDL Cholesterol: Understanding the “Bad” and Aiming for Optimal
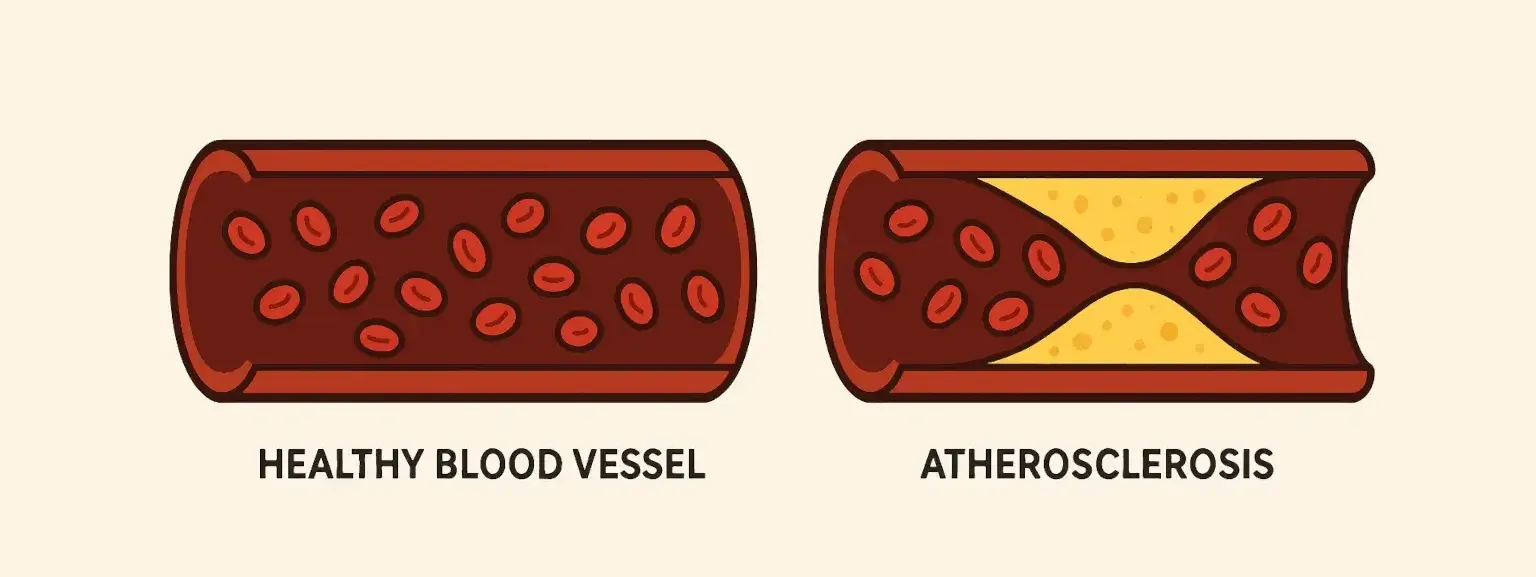
Low-Density Lipoprotein (LDL) cholesterol is often labeled ‘bad’ cholesterol because elevated levels are a primary driver of atherosclerosis—the buildup of fatty plaques in artery walls [2]. This process can narrow arteries, restrict blood flow, and ultimately lead to heart attacks or strokes. Thus, managing LDL cholesterol is a critical aspect of preventive cardiology.
Optimal LDL cholesterol levels are personalized based on an individual’s overall cardiovascular risk. European guidelines, for instance, advocate for LDL levels below 55 mg/dL (1.4 mmol/L) for very high-risk individuals, such as those with existing cardiovascular disease or diabetes [3], [1]. The American Heart Association (AHA) generally recommends an LDL target below 100 mg/dL (2.6 mmol/L) for the general population, with a stricter target of below 70 mg/dL (1.8 mmol/L) for those at higher risk [4]. Compelling clinical trial evidence shows that lowering LDL cholesterol, particularly to levels below 70 mg/dL, can stabilize arterial plaques and markedly reduce cardiovascular events [4].
Strategies for Lowering LDL:
- Pharmacological Interventions: Statins are the first-line medication, inhibiting cholesterol production in the liver and offering anti-inflammatory benefits [5]. For individuals who cannot reach their LDL goals with statins or experience side effects, other options include ezetimibe (inhibits cholesterol absorption) and potent injectable PCSK9 inhibitors (e.g., alirocumab, evolocumab), which can lower LDL to very low levels. A newer option, inclisiran, is a small interfering RNA (siRNA) therapy administered twice a year, also targeting PCSK9 [5].
- Lifestyle Modifications: These are fundamental. Adopting a heart-healthy dietary pattern, such as the Mediterranean or DASH diet, rich in fruits, vegetables, whole grains, and unsaturated fats, is crucial for reducing saturated and trans fat intake [6]. Regular physical activity, weight management, and smoking cessation are also vital for improving lipid profiles and overall cardiovascular health [2].
While the benefits of lowering LDL are clear, the discussion continues on the optimal balance between medication and lifestyle changes. Personalized medicine, incorporating comprehensive risk assessments including tools like CT-based calcium scoring, helps tailor interventions effectively [4]. Understanding your lipid panel for longevity involves a proactive approach to LDL management.
HDL Cholesterol: Beyond Just “Good” Cholesterol
 High-Density Lipoprotein (HDL) cholesterol is traditionally known as “good” cholesterol due to its role in reverse cholesterol transport—removing excess cholesterol from arteries and transporting it to the liver for processing or excretion [2]. Higher HDL levels have historically been linked to lower cardiovascular risk.
High-Density Lipoprotein (HDL) cholesterol is traditionally known as “good” cholesterol due to its role in reverse cholesterol transport—removing excess cholesterol from arteries and transporting it to the liver for processing or excretion [2]. Higher HDL levels have historically been linked to lower cardiovascular risk.
However, the narrative around HDL has become more nuanced. Simply having high HDL levels doesn’t guarantee protection, and clinical trials of drugs designed solely to raise HDL cholesterol have not consistently resulted in reduced cardiac events [4]. This suggests that HDL function—its efficiency in tasks like cholesterol efflux, anti-inflammatory, and antioxidant activities—may be more important than its concentration alone.
Influencing HDL Positively:
- Exercise: Aerobic exercise is a proven way to modestly increase HDL cholesterol levels. Meta-analyses indicate that structured aerobic training can raise HDL-C, with longer duration and intensity potentially yielding greater benefits [7].
- Gender Considerations: Hormonal differences influence HDL levels. Men tend to have lower HDL levels than premenopausal women. After menopause, women’s HDL levels may decrease [8].
The focus is shifting from merely elevating HDL levels to promoting overall HDL functionality through healthy lifestyle choices. So, is high HDL always good for you? The answer is complex; it’s one part of a larger metabolic picture.
Lipoprotein(a): The Genetic Risk Factor You Need to Know
Lipoprotein(a), or Lp(a), is an LDL-like particle with an additional protein called apolipoprotein(a) attached. Elevated Lp(a) is a significant, largely genetically determined, independent risk factor for atherosclerotic cardiovascular disease (ASCVD), including heart attack, stroke, and aortic stenosis [9], [10]. Because Lp(a) levels are set by your genes and remain relatively stable throughout life, a single blood test can determine your level [4].
Lp(a) contributes to cardiovascular risk by promoting plaque buildup, inflammation, and clotting [9]. Unlike other lipoproteins, Lp(a) levels are not significantly affected by lifestyle changes or most standard cholesterol-lowering drugs.
Understanding and Addressing Lp(a):
- Population Variability: Lp(a) levels vary considerably across different ancestral groups, with individuals of African descent generally having the highest levels. However, the relative risk increase per unit of Lp(a) is similar across ancestries [10].
- Risk Assessment: An Lp(a) level above 50 mg/dL (or approximately 125 nmol/L) is generally considered to confer increased risk, though specific thresholds can vary [10]. Mendelian randomization studies confirm a causal link between high Lp(a) and increased risk of coronary artery disease and peripheral artery disease [11].
- Emerging Therapies: This is an exciting area of research. Antisense oligonucleotides (e.g., pelacarsen) and small interfering RNA (siRNA) therapies (e.g., lepodisiran) are designed to specifically lower Lp(a) production by the liver. Lepodisiran, for example, has shown the ability to reduce Lp(a) levels by over 90% in clinical trials, with effects lasting up to a year [12]. These treatments offer hope for individuals with high genetic Lp(a) risk.
Lp(a) genetic testing and cardiovascular risk assessment are becoming more critical in personalized preventive cardiology.
Apolipoprotein B (ApoB): The True Count of Risky Particles
Apolipoprotein B (apoB) is a protein found on all the “bad” atherogenic (plaque-forming) lipoproteins: LDL, VLDL (very-low-density lipoprotein), IDL (intermediate-density lipoprotein), and Lp(a). Each of these particles contains exactly one molecule of apoB. Therefore, measuring apoB provides a direct count of the total number of these potentially harmful particles circulating in your blood [13].
Many experts consider apoB a more accurate and comprehensive indicator of cardiovascular risk than LDL cholesterol (LDL-C) alone. This is especially true in individuals with conditions like metabolic syndrome, type 2 diabetes, or very low LDL-C levels, where LDL-C might underestimate the actual number of atherogenic particles [13].
Why ApoB Matters for Longevity:
- Comprehensive Risk Assessment: An optimal apoB level is generally considered to be less than 80 mg/dL for the general population, with lower targets for higher-risk individuals, aligning with aggressive LDL management strategies [14].
- Guiding Therapy: Tracking apoB can help ensure that therapies are adequately reducing the total burden of atherogenic particles, thus playing a key role in preventing heart disease.
Integrating apoB measurement into routine lipid panels offers a more refined approach to cardiovascular risk stratification and management.
| Human plasma apolipoproteins | |||
|---|---|---|---|
| apolipoprotein | molecular weight | lipoprotein distribution | |
| apoA-I | 28,331 | HDL | |
| apoA-II | 17,380 | HDL | |
| apoB-48 | 241,000 | chylomicrons | |
| apoB-100 | 500,000 | VLDL, LDL | |
| apoC-I | 7,000 | HDL, VLDL | |
| apoC-II | 8,837 | chylomicrons, VLDL, HDL | |
| apoC-III | 8,750 | chylomicrons, VLDL, HDL | |
| apoD | 33,000 | HDL | |
| apoE | 34,145 | chylomicrons, VLDL, HDL | |
| Source: From Dennis E. Vance andJean E. Vance, Biochemistry of Lipids and Membranes(1985), Table 13.4. |
Summary Table: Optimal Lipoprotein Levels for Longevity and Healthspan
| Lipoprotein | Optimal Level (mg/dL unless stated) | Key Considerations for Healthspan |
|---|---|---|
| LDL Cholesterol | <100 (general); <70 or <55 (high/very high risk) | Lowering LDL is a cornerstone of CVD prevention; “lower is better” for high-risk individuals. [1], [3] |
| HDL Cholesterol | >40 (men), >50 (women) | Focus on function and healthy lifestyle; high levels alone don’t guarantee protection. [4] |
| Lipoprotein(a) [Lp(a)] | <30 mg/dL or <75 nmol/L (desirable); >50 mg/dL or >125 nmol/L (high risk) | Genetically determined; important independent risk factor. Emerging therapies show promise. [10] |
| Apolipoprotein B (ApoB) | <80 (general); <65 (high risk) | Reflects total number of atherogenic particles; may be a better risk marker than LDL-C alone. [13] |
Note: Optimal levels can vary based on individual risk profiles and specific guideline recommendations. Discuss your specific targets with your healthcare provider.
Conclusion: Integrating Lipoprotein Management for Enhanced Longevity
Effectively managing your lipoprotein profile is a powerful strategy for enhancing both longevity and healthspan. This involves a comprehensive understanding of not just LDL and HDL, but also the increasingly recognized roles of Lp(a) and apoB.
A proactive approach should include:
- Regular Screening: Know your numbers through advanced lipid testing.
- Lifestyle Optimization: Prioritize a heart-healthy diet, consistent physical activity, healthy weight, and avoiding tobacco. [6]
- Personalized Medical Management: Work with your healthcare provider to determine if medications are needed to reach optimal lipoprotein targets, especially if you have high LDL, high Lp(a), or elevated apoB.
By embracing these evidence-based strategies, we can take significant strides in mitigating cardiovascular risk, paving the way for a longer, healthier, and more fulfilling life. Future research will continue to refine our understanding and treatment options, making personalized lipoprotein management an even more potent tool for longevity.
Frequently Asked Questions (Q&A)
Q1: What do LDL and HDL cholesterol mean for my health?
Q2: Why is Lipoprotein(a) important if it's genetic?
Q3: What is apoB, and why might it be a better marker than LDL cholesterol?
Q4: What are the most effective lifestyle changes to improve my lipoprotein profile?
Q5: Are there new treatments for managing high cholesterol and Lp(a)?
Disclaimer
The information provided on BioBrain is intended for educational purposes only and is grounded in science, common sense, and evidence-based medicine. It is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider before making significant changes to your diet, exercise routine, or overall health plan.
References
- Harvard Medical School (2021) "How low should your LDL cholesterol go?"
- Centers for Disease Control and Prevention (CDC) (2024) "LDL & HDL Cholesterol & Triglycerides"
- Mach F, Baigent C, Catapano AL, et al. (2020) "2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk"
- Mass General Brigham (2023) "What are healthy cholesterol levels?"
- UCLA Health (2023) "Injectable medications prove effective at lowering LDL ‘bad’ cholesterol"
- National Heart, Lung, and Blood Institute (NHLBI) (2022) "Manage Cholesterol"
- Ferguson JH, et al. (2024) "The Effects of Exercise Training on High-Density Lipoprotein Cholesterol: A Systematic Review and Meta-Analysis of Randomized Controlled Trials"
- American Heart Association (2020) "What Your Cholesterol Levels Mean"
- Tsimikas S (2017) "A Test in Context: Lipoprotein(a): Diagnosis, Prognosis, Controversies, and Emerging Therapies"
- Kronenberg F, Mora S, Stroes ESG, et al. (2022) "Lipoprotein(a) in atherosclerotic cardiovascular disease and aortic stenosis: a European Atherosclerosis Society consensus statement"
- Gudmundsdottir V, et al. (2024) "Lipoprotein(a) levels and risk of peripheral artery disease and coronary artery disease: a Mendelian randomization study"
- Nissen SE, et al. (2024) "Lepodisiran, an Extended-Duration siRNA Targeting Lipoprotein(a): A Randomized Dose-Finding Clinical Trial"
- Sniderman AD, Thanassoulis G, Glavinovic T, et al. (2019) "Apolipoprotein B Particles and Cardiovascular Disease: A Narrative Review"
- American Heart Association "Cholesterol Medications"
Tags :
- Ldl cholesterol
- Hdl cholesterol
- Lipoprotein(a)
- Apolipoprotein b
- Healthspan
- Lifespan
- Cardiovascular health
- Longevity science
- Cholesterol management
- Lipid panel
- Optimize lipoproteins for longevity
- Understanding lipid panel for longevity
- Lp(a) genetic risk
- Apo b heart disease prevention